Adult Pulmonary Conditions
All CCPC pulmonary physicians have undergone subspeciality training and are board certified in pulmonary diseases. Our specialty clinics offer comprehensive care to persons with pulmonary disorders including:
ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS)
Acute Respiratory Distress Syndrome (ARDS) is a life-threatening problem in which the lungs are severely injured. Inflammation (swelling) occurs throughout the lungs. In the lung tissue, tiny blood vessels leak fluid and the air sacs (alveoli) collapse or fill with fluid. This fluid buildup keeps the lungs from working well. Persons with this problem will have trouble bringing enough oxygen in and removing carbon dioxide from the body, and become short of breath. Persons with ARDS must be given extra oxygen and will usually need the help of a mechanical ventilator (respirator) to breathe. With medical care, many people with ARDS survive and recover. However, up to 40% of people with ARDS die from the syndrome, even with intensive treatment.
ALPHA-1 ANTITRYPSIN DEFICIENCY
Alpha-1 antitrypsin deficiency is an inherited form of emphysema (em-fuh-ZEE-muh). People with this condition, also known as AAT deficiency, do not have enough of a protein called alpha-1 antitrypsin (AAT) in their blood. This protein is made in the liver, and it protects the lungs so they can work normally. Without enough AAT, the lungs can become damaged by emphysema. AAT deficiency can also cause liver damage.
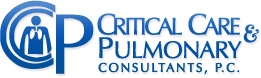
ASTHMA
Asthma is a chronic disease that cannot be cured. However, it does not cause permanent damage to the lungs and with daily care it can be controlled. Deaths from asthma are rare, usually preventable, and most commonly caused by a lack of medical care and improper use of medicines. Many patients wonder if asthma can evolve into emphysema. Emphysema is a different disease that is common among individuals who smoke, but does not evolve from asthma. With emphysema, there is permanent lung damage in the alveoli. Some people who smoke have both asthma and emphysema.
No one knows what causes asthma, but more people are developing it. However while you have no power over the fact you have asthma, you have the ability to control the disease. When asthma is controlled, the condition of your lungs returns to normal. It is important that you take care of yourself and see your doctor on a regular basis so an asthma control plan can be developed. Once you have a plan, you will only need to spend a few minutes each day to monitor and control your disease. Exercise, proper diet and adequate sleep are important in living a healthy life for all of us. If you keep your asthma under control, you will be able to perform most of your usual activities and exercises.
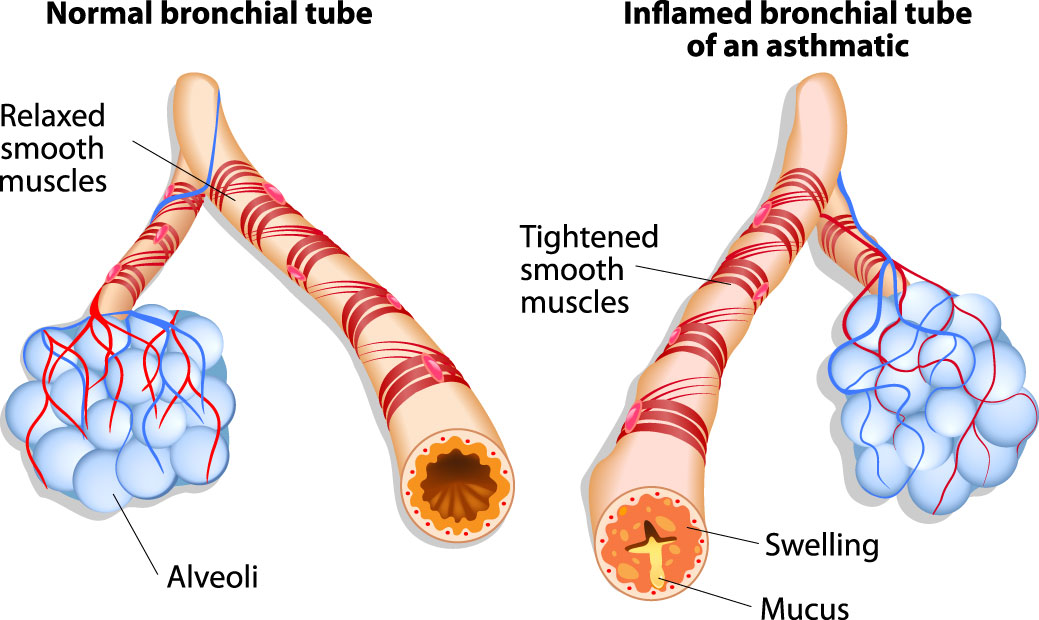
BRONCHITIS
When you breathe in, the air travels down through your trachea (windpipe). It then goes through two tubes to your lungs. These tubes are your bronchi. Bronchial disorders can make it hard for you to breathe. The most common problem with the bronchi is bronchitis, an inflammation of the tubes. It can be acute or chronic.
Chronic bronchitis is one type of COPD. The inflamed bronchial tubes produce a lot of mucus. This leads to coughing and difficulty breathing. Cigarette smoking is the most common cause. Breathing in air pollution, fumes, or dust over a long period of time may also cause it. To diagnose chronic bronchitis, your doctor will look at your signs and symptoms and listen to your breathing. You may also have other tests. Chronic bronchitis is a long-term condition that keeps coming back or never goes away completely.
Other problems associated with bronchitis include:
- Bronchiectasis – a condition in which damage to the airways causes them to widen and become flabby and scarred
- Exercise-induced bronchospasm – a breathing problem that happens when your airways shrink while you are exercising
- Bronchiolitis – an inflammation of the small airways that branch off from the bronchi
- Bronchopulmonary dysplasia – a chronic lung condition in infants, most often premature infants
Source: MedlinePlus, National Library of Medicine
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)
Chronic Obstructive Pulmonary Disease (COPD) is a preventable and treatable disease that makes it difficult to empty air out of the lungs. This can lead to shortness of breath or feeling tired because you are working harder to breathe. In general, COPD is a term that is used to include chronic bronchitis, emphysema, or a combination of both conditions. Asthma is also a disease where it is difficult to empty the air out of the lungs, but asthma is not included in the definition of COPD. It is not uncommon, however for a patient with COPD to also have some degree of asthma.
COPD: SIGNS AND SYMPTOMS
COPD may cause shortness of breath, tiredness, production of mucus, and cough. Many people with COPD develop most, if not all, of these signs and symptoms.
COPD: MEDICATIONS USED FOR TREATMENT
The most common medications for treating COPD are bronchodilators and steroids. Both make breathing easier, but do so in different ways.
COPD: OXYGEN THERAPY
Patients with lung disease can have low levels of oxygen in their bodies and some need to use extra (supplemental) oxygen to achieve healthier oxygen levels. Adults and children with lung diseases such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, cystic fibrosis (CF), or bronchopulmonary dysplasia (BPD) may require this therapy. Extra oxygen protects their bodies from the effects of low oxygen levels, helps them to function better, and allows them to stay more active.
COPD: SURGERY FOR CHRONIC OBSTRUCTIVE PULMONARY DISEASE
If you have COPD, you may benefit from lung surgery. However, only a small number of people have the type of COPD that will benefit from surgery. The major types of surgery for COPD are bullectomy, lung volume reduction (LVRS) and lung transplantation. If you have COPD and require surgery for other reasons, you should speak with your healthcare provider before having any operation.
COPD: USING YOUR NEW INHALER WITH HFA PROPELLANT
If you have a lung disease such as COPD or asthma, you are probably using an inhaler. There are several different types of inhalers, all of which deliver medicine into your lungs. However, if you have never been taught to use your inhaler correctly, then you may not be getting the full benefit of your inhaled medicine. At your next visit with your healthcare provider, bring your inhaler(s) and ask them to check that you are using them correctly.
CHRONIC COUGH
Coughing is a reflex that keeps your throat and airways clear. Although it can be annoying, coughing helps your body heal or protect itself. Coughs can be either acute or chronic. Acute coughs begin suddenly and usually last no more than 2 to 3 weeks. Acute coughs are the kind you most often get with a cold, flu, or acute bronchitis. Chronic coughs last longer than 2 to 3 weeks. Causes of chronic cough include
- Chronic bronchitis
- Asthma
- Allergies
- COPD (chronic obstructive pulmonary disease)
- GERD (gastroesophageal reflux disease)
- Smoking
- Throat disorders, such as croup in young children
- Some medicines
Water can help ease your cough – whether you drink it or add it to the air with a steamy shower or vaporizer. If you have a cold or the flu, antihistamines may work better than non-prescription cough medicines. Children under four should not have cough medicine. For children over four, use caution and read labels carefully.
Source: MedlinePlus, National Library of Medicine.
EMPHYSEMA
Emphysema is a type of COPD involving damage to the air sacs (alveoli) in the lungs. As a result, your body does not get the oxygen it needs. Emphysema makes it hard to catch your breath. You may also have a chronic cough and have trouble breathing during exercise.
The most common cause is cigarette smoking. If you smoke, quitting can help prevent you from getting the disease. If you already have emphysema, not smoking might keep it from getting worse. Treatment is based on whether your symptoms are mild, moderate or severe. Treatments include inhalers, oxygen, medications and sometimes surgery to relieve symptoms and prevent complications.
Source: MedlinePlus, National Library of Medicine.
INTERSTITIAL LUNG DISEASE
Interstitial lung disease is the name for a large group of diseases that inflame or scar the lungs. The inflammation and scarring make it hard to get enough oxygen. The scarring is called pulmonary fibrosis. Breathing in dust or other particles in the air is responsible for some types of interstitial lung diseases. Specific types include:
- Black lung disease among coal miners, from inhaling coal dust
- Farmer’s lung, from inhaling farm dust
- Asbestosis, from inhaling asbestos fibers
- Siderosis, from inhaling iron from mines or welding fumes
- Silicosis, from inhaling silica dust
Other causes include autoimmune diseases or occupational exposures to molds, gases, or fumes. Some types of interstitial lung disease have no known cause. Treatment depends on the type of exposure and the stage of the disease. It may involve medicines, oxygen therapy, or a lung transplant in severe cases.
Source: MedlinePlus, National Library of Medicine.
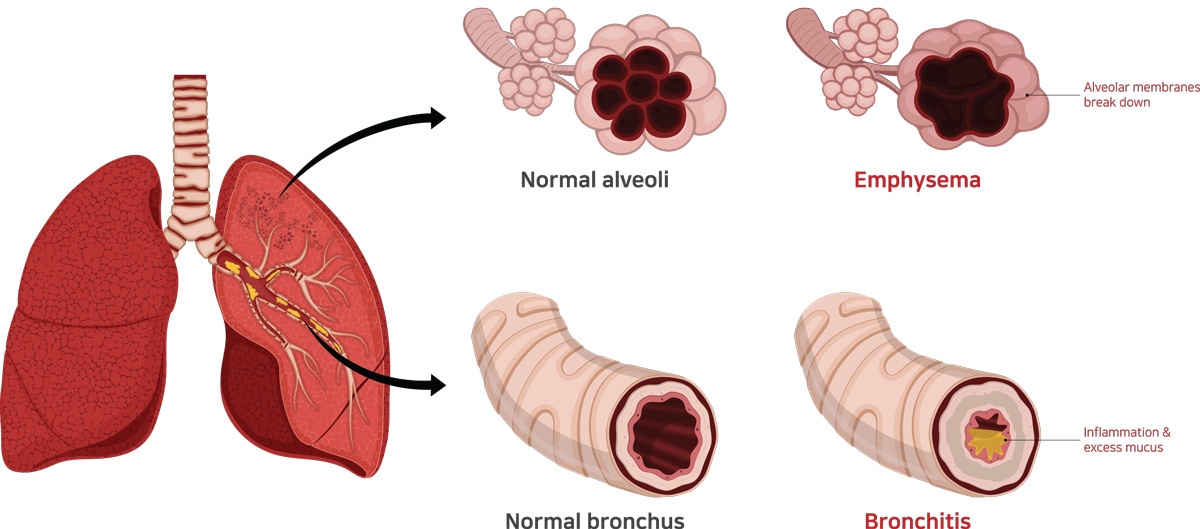
LUNG CANCER
Lung cancer is an abnormal, uncontrolled growth of cells within the lung. Lung cancer is the leading cause of cancer deaths in the United States and will cause more deaths this year than cancer of the breast, prostate and colon combined.
LUNG CANCER: SCREENING
Lung cancer screening in a specific group of patients has been shown to decrease mortality (death). If you smoke cigarettes, or quit smoking less than 15 years ago, and are between the ages of 55 to 80, you may be a candidate for lung cancer screening. If you have questions about lung cancer screening or think you may be a candidate, please ask your doctor for more information.
LUNG CANCER: FIBEROPTIC BRONCHOSCOPY
Fiberoptic bronchoscopy (bron-kos’ko-pi) is a visual exam of the breathing passages of the lungs (called “airways”). This test is done when it is important for your doctor to see inside the airways of your lungs, or to get samples of mucus or tissue from the lungs. Bronchoscopy involves placing a thin tube-like instrument called a bronchoscope (bron’ko-sko-p) through the nose or mouth and down into the airways of the lungs. The tube has a mini-camera at its tip, and is able to carry pictures back to a video screen or camera. Bronchoscopy is sometime done with an ultrasound probe (EBUS or endobronchial ultrasound) to better visualize and biopsy structures such as lymph nodes. Navigational bronchoscopy uses state of the art technology to more precisely localize and biopsy small lung lesions.
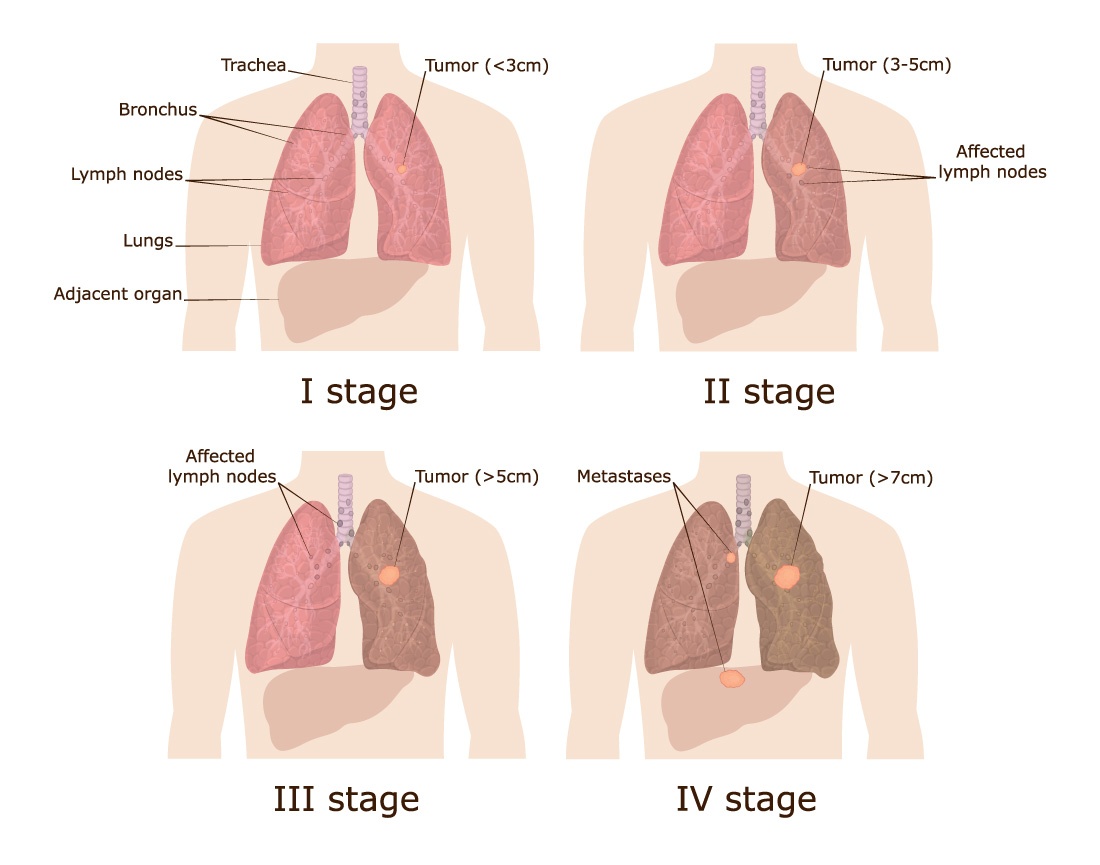
LUNG CANCER: STAGING
Once your lung cancer is diagnosed, staging tells you and your healthcare provider about the size of your cancer (tumor) and how far it has spread. The stage of your cancer is based on your symptoms, results from tests like a CT scan (also called a cat scan) or PET scan, and biopsies. A biopsy involves removing a piece of tissue, usually from your lung or lymph node, and looking at it under a microscope. The stages of lung cancer are listed as I, II, III, and IV for non-small cell lung cancer and “limited” or “extensive” for small cell lung cancer. The higher the number (or when the word “extensive” is used) means the bigger the tumor and/or the more the cancer has spread.
LYMPHANGIOLEIOMYOMATOSIS (LAM)
Lymphangioleiomyomatosis (lim-FAN-jee-oh-ly-oh-myoh-ma-TOE-sis), commonly known as LAM, is a rare lung disease that affects women almost exclusively, usually during their childbearing years. People with LAM have an unusual type of muscle cell that grows in the tissues of the lungs. Although these cells are not considered cancerous, they grow uncontrollably throughout the lungs. These muscle cells can block the lymph vessels, blood vessels, and airways, preventing the lungs from providing oxygen to the rest of the body.
OCCUPATIONAL LUNG DISEASES
Occupational lung diseases are caused or made worse by your work environment. They occur from inhaling dusts, chemicals, bacteria, or mold at work. It is important to know about these lung diseases because they can be prevented or kept from getting worse. The major groups of occupational lung diseases are:
- Work-related asthma
- Lung disease from dusts and metals
- Allergic problems
- Reactions from irritants
- Lung or other cancers
- Infections
PNEUMONIA
Pneumonia is an infection in one or both of the lungs. Many germs, such as bacteria, viruses, and fungi, can cause pneumonia. You can also get pneumonia by inhaling a liquid or chemical. People most at risk are older than 65 or younger than 2 years of age, or already have health problems.
Symptoms of pneumonia vary from mild to severe. See your doctor promptly if you
- Have a high fever
- Have shaking chills
- Have a cough with phlegm that doesn’t improve or gets worse
- Develop shortness of breath with normal daily activities
- Have chest pain when you breathe or cough
- Feel suddenly worse after a cold or the flu
Your doctor will use your medical history, a physical exam, and lab tests to diagnose pneumonia. Treatment depends on what kind you have. If bacteria are the cause, antibiotics should help. If you have viral pneumonia, your doctor may prescribe an antiviral medicine to treat it.
Preventing pneumonia is always better than treating it. Vaccines are available to prevent pneumococcal pneumonia and the flu. Other preventive measures include washing your hands frequently and not smoking.
Source: MedlinePlus, National Library of Medicine.
PULMONARY FIBROSIS
Pulmonary fibrosis is a condition in which the tissue deep in your lungs becomes scarred over time. This tissue gets thick and stiff. That makes it hard for you to catch your breath, and your blood may not get enough oxygen.
Causes of pulmonary fibrosis include environmental pollutants, some medicines, some connective tissue diseases, and interstitial lung disease. Interstitial lung disease is the name for a large group of diseases that inflame or scar the lungs. In most cases, the cause cannot be found. This is called idiopathic pulmonary fibrosis.
Symptoms include:
- Shortness of breath
- A dry, hacking cough that doesn’t get better
- Fatigue
- Weight loss for no known reason
- Aching muscles and joints
- Clubbing, which is the widening and rounding of the tips of the fingers or toes
Your doctor may use your medical history, imaging tests, a biopsy, and lung function tests to diagnose pulmonary fibrosis. There is no cure. Treatments can help with symptoms and improve your quality of life. They include medicines, oxygen therapy, pulmonary rehabilitation, or a lung transplant.
Source: MedlinePlus, National Library of Medicine.
PULMONARY HYPERTENSION
Pulmonary hypertension (PH) is high blood pressure in the arteries to your lungs. It is a serious condition. If you have it, the blood vessels that carry blood from your heart to your lungs become hard and narrow. Your heart has to work harder to pump the blood through. Over time, your heart weakens and cannot do its job and you can develop heart failure.
Symptoms of PH include
- Shortness of breath during routine activity, such as climbing two flights of stairs
- Tiredness
- Chest pain
- A racing heartbeat
- Pain on the upper right side of the abdomen
- Decreased appetite
As PH worsens, you may find it hard to do any physical activities.
There are two main kinds of PH. One runs in families or appears for no known reason. The other kind is related to another condition, usually heart or lung disease.
There is no cure for PH. Treatments can control symptoms. They involve treating the heart or lung disease, medicines, oxygen, and sometimes lung transplantation.
Source: MedlinePlus, National Library of Medicine.
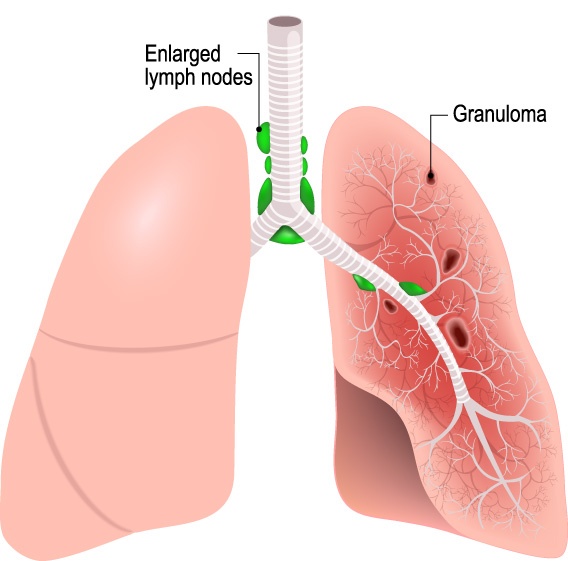
SARCOIDOSIS
Sarcoidosis (sar-coy-DOE-sis) is a disease in which inflammation produces tiny lumps of cells in organs throughout the body. The lumps, called granulomas, most often appear in the lungs, but they can also occur in the lymph nodes, eyes, skin, or other areas of the body. If these tiny lumps grow in an organ, they can affect how well the organ works. When sarcoidosis affects the lungs (pulmonary sarcoidosis), the disease can reduce the lung capacity, cause abnormal stiffness of the lungs, and cause breathing problems.
VOCAL CORD DYSFUNCTION (VCD)
Vocal Cord Dysfunction means that your vocal cords do not act normally. With VCD, instead of your vocal cords opening when you breathe in and out, your vocal cords tend to close. When your vocal cords close, it makes it harder to get air into or out of your lungs. People with vocal cord dysfunction may have symptoms of cough, shortness of breath, or wheezing. Sometimes vocal cord dysfunction can be mistaken for asthma.